NHS 111
If you need medical help fast, but it’s not a 999 emergency; or you want advice about treating your child's symptoms at home; or you need to access a local medical service but you're not sure which one, start with NHS 111.
NHS 111 is available 24 hours a day, 365 days a year. Visit the NHS 111 website or call 111 free from your landline or mobile phone.
Trained advisors will ask you a series of questions to assess your child’s symptoms and then if necessary, book an appointment for you to attend the local healthcare service that’s right for them. If the NHS 111 team think you need an ambulance, they will send one immediately.
Pharmacies
Pharmacists are trained medicine experts who can give you advice on treating a range of common childhood conditions and minor injuries such as:
- sore throat
- coughs
- colds and flu
- insect bites
- earache
- skin rashes
You don't need to make an appointment to visit your local pharmacist, and many pharmacies are open during the evening and at weekends. Find your nearest pharmacy.
HANDi App
Parents, carers and healthcare professionals can access expert advice about common childhood illnesses and how to treat them via a free mobile app, called HANDi App.
Developed and approved by Paediatric Consultants at the Royal United Hospital (RUH), the HANDi App provides expert advice on how best to manage the six most common childhood illnesses; diarrhoea and vomiting, high temperature, chestiness, newborn problems and stomach pain. The HANDi App aims to give parents and carers more confidence in dealing with minor conditions at home.
It's easy to use as it takes the user through a series of questions about the symptoms their child is experiencing and then advises on the best course of action, whether that's to treat at home, make a GP appointment or to go to A&E.
Bath and Wiltshire residents can search for 'HANDi App' in their app store to download it.
To find out more about the HANDi App, visit the RUH website.
Useful links
When Should I worry Booklet (available in multiple languages)
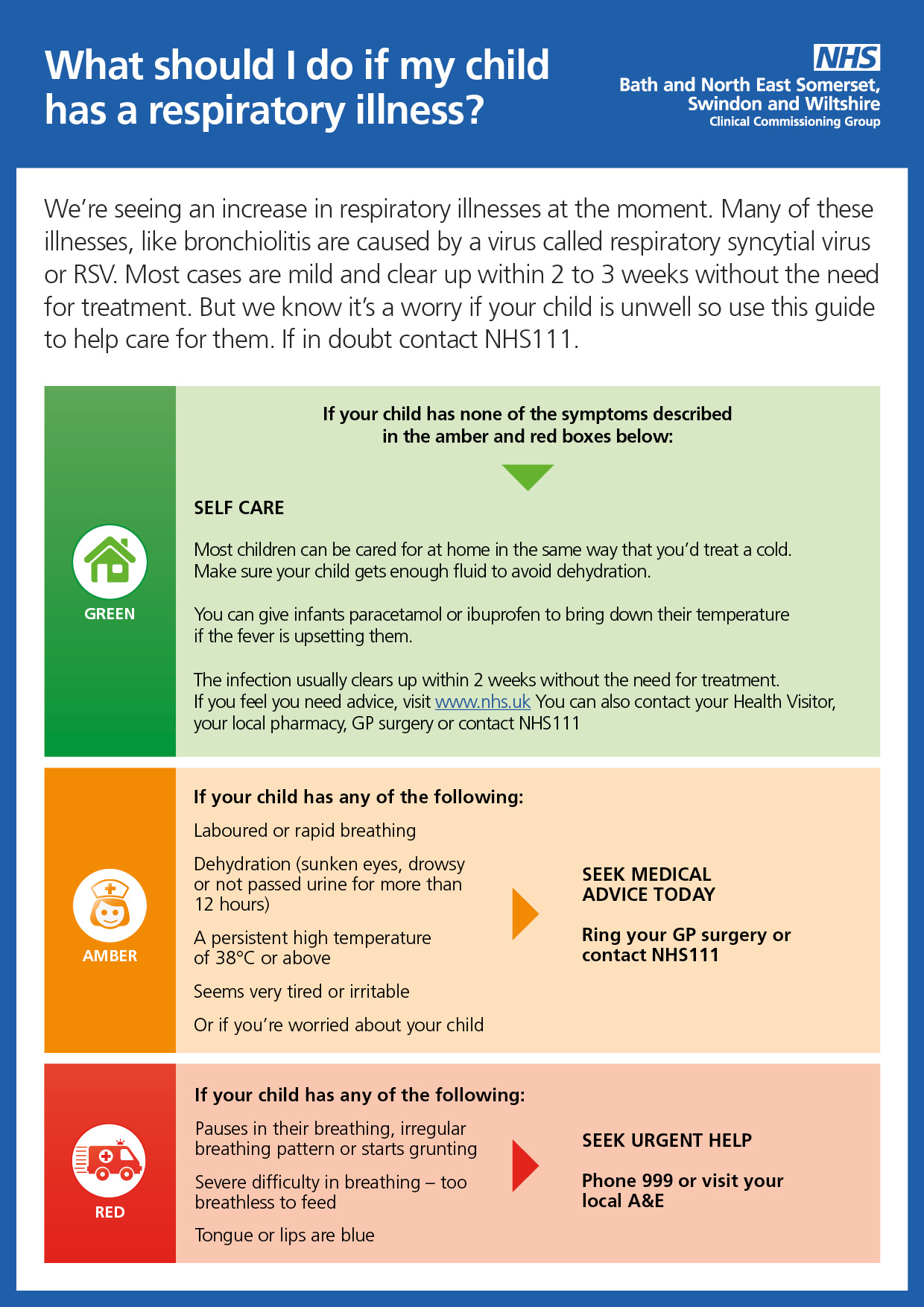
Respiratory illness in children